KNEE PROSTHESIS - TOTAL KNEE ARTHROPLASTY (TKA)
Major innovations have been made in the orthopedic science during the past decades. Material for implants have been significantly improved, surgical techniques have been fine-tuned, advanced software and robots are commonly utilized into the surgery room. Therefore, TKA surgeries have now a high level of success rate.
60,000 TKA are performed each year in France. In most cases, the TKA is performed because of a severe arthrosis pathology occurs : 40% of people over 60 are suffering of arthrosis. Hopefully not all these people will have to get a knee surgery.
The knee prosthesis can be either unicompartmental or total knee arthrosplasty. They are chosen by your surgeon depending on the arthrosis you have. To make this choice, your surgeon will analyze your X-ray images.
60,000 TKA are performed each year in France. In most cases, the TKA is performed because of a severe arthrosis pathology occurs : 40% of people over 60 are suffering of arthrosis. Hopefully not all these people will have to get a knee surgery.
The knee prosthesis can be either unicompartmental or total knee arthrosplasty. They are chosen by your surgeon depending on the arthrosis you have. To make this choice, your surgeon will analyze your X-ray images.
DO I NEED A KNEE REPLACEMENT ?
This key question will pop up when :
• Your knee is so painful that you feel a permanent discomfort. This pain significantly changes your quality of life, at home, at your job or when you’re practicing sports.
• Drug treatments or injections are not effective anymore, or these treatments have bad side-effects, or these treatments put your health at risk because of future complications.
You are the only one who is making this key decision, your surgeon is only your advisor to help you validating or not the TKA option.
If the above symptoms are clearly present, don’t waste time ! You have to get a TKA as soon as possible because the stiffness will get worse and your muscles will get weaker. And you will need your muscles in good shape to reduce your recovery time.
TKA patients who have waited too long always thank their surgeon to get it done and say “If I had known, I would have done it before...!”
• Your knee is so painful that you feel a permanent discomfort. This pain significantly changes your quality of life, at home, at your job or when you’re practicing sports.
• Drug treatments or injections are not effective anymore, or these treatments have bad side-effects, or these treatments put your health at risk because of future complications.
You are the only one who is making this key decision, your surgeon is only your advisor to help you validating or not the TKA option.
If the above symptoms are clearly present, don’t waste time ! You have to get a TKA as soon as possible because the stiffness will get worse and your muscles will get weaker. And you will need your muscles in good shape to reduce your recovery time.
TKA patients who have waited too long always thank their surgeon to get it done and say “If I had known, I would have done it before...!”
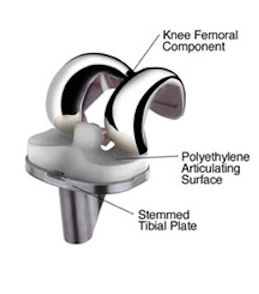
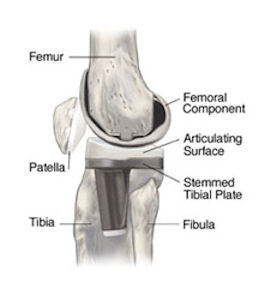
WHAT ARE THE COMPONANTS OF A KNEE PROSTHESIS ?
In a TKA surgery, all parts of your joint are replaced by artificial components.
In most cases, these materials are composed of :
Each patient will have a specific implant in terms of size, shape, material types, coating types and will have a specific surgical technique.
The associated components can be attached with surgical cement or not.
In some very rare cases, patients could experience allergies to some metal components, such as Cobalt. If you know that you are cobalt sensitive or other metals sensitive, you must mention these allergies when we meet each other. In that case, there are other options for your implant. You can click here to see the chemical components utilized to manufacture the implants I’m using.
The prosthesis stability is secured thanks to the ligaments and the tendons that connect muscles to bones, especially the extensor muscles with the quadriceps, the patella and the patellar tendon. Therefore, it is very critical to avoid any damage of these soft tissues : the mini-intrusive surgical techniques enable us to significantly reduce these risks.
The average lifetime of knee prosthesis is roughly 15 to 20 years. This lifetime depends on the usage level of the implant with regards of the physical activities of your knee.
You could get further information on the implant I’m using by clicking here.
In most cases, these materials are composed of :
- metal parts, to replace the cartilage parts (so-called “surfacing”)
- poly-ethylene parts in between metal parts.
Each patient will have a specific implant in terms of size, shape, material types, coating types and will have a specific surgical technique.
The associated components can be attached with surgical cement or not.
In some very rare cases, patients could experience allergies to some metal components, such as Cobalt. If you know that you are cobalt sensitive or other metals sensitive, you must mention these allergies when we meet each other. In that case, there are other options for your implant. You can click here to see the chemical components utilized to manufacture the implants I’m using.
The prosthesis stability is secured thanks to the ligaments and the tendons that connect muscles to bones, especially the extensor muscles with the quadriceps, the patella and the patellar tendon. Therefore, it is very critical to avoid any damage of these soft tissues : the mini-intrusive surgical techniques enable us to significantly reduce these risks.
The average lifetime of knee prosthesis is roughly 15 to 20 years. This lifetime depends on the usage level of the implant with regards of the physical activities of your knee.
You could get further information on the implant I’m using by clicking here.
SOME TECHNICAL INPUT
MINI-INVASIVE SURGERY
This innovative technique has been developed in USA. Surgeons like me have an international certification with on-going updates and training to be able to practice it. This technique enables to reduce the incision length by 50% and to protect the soft tissues around the knee joint when a TKA is performed. I’m extensively using this advanced technique.Other benefits are the blood loss reduction during the surgery, less pain right after the surgery, a reduction of the length of stay at the hospital and a reduction of the recovery period. I’m using this technique for a wide majority of my patients.
COMPUTER ASSISTED SURGERY
I started to use computer aided surgery in 1999 when robots started to be utilized in the surgery room with "CASPAR" (Computer Assisted Surgery Planning And Robotic). Since then, this technology has been refined and I’m using advanced new software and hardware technologies during my surgeries: I’m a member of the International society for Computer Assisted Orthopedic Surgery) : this membership provides me with the latest innovation and state of the art surgical techniques.This Computer Assisted Surgery enables to perfectly control the prosthesis localization by double-checking all implant component positioning. This technique is so-called “computer surgical navigation”.
PATIENT SPECIFIC INSTRUMENTATION
In some cases, I will use a custom-made ancillary tool : this is a tool to align and perfectly position the prosthesis. To do so, you will need to get a scan or an IRM of your knee before the surgery, to manufacture your ancillary-tools. This step takes about 6 weeks. I have used this specific technique since 2008.ENHANCED RECOVERY AFTER SURGERY (ERAS)
This new care pathways enables to reduce your hospital stay to the minimum time length (0 to 2 days) and to start your recovery right after your surgery. Then, you will be able to get back home by your own. This ERAS technique is a clear revolution in the way patients are experiencing an orthopedic surgery. This technique is a real breakthrough and a complete section of this website is available to explain all the benefits of ERAS technique. You can click : Enhanced Recovery After Surgery (ERAS).On a regular basis, I’m a lecturer and I’m giving keynotes and conferences to surgeons to explain the ERAAS technique and its benefits.
I’m also training other orthopedic surgeons about how to apply ERAS process within the hip and knee arthroplasty surgery.
AMBULATORY SURGERY
I’ve been practicing this ambulatory knee or hip surgery on a regular basis since July 2016. This specific care pathways enables the patient to get back home the day of the surgery. This technique has been broadly deployed in USA. Today, 2 patients out of 3 for hip prosthesis and 1 patient out of 2 for knee prosthesis can benefit from this technique.There is now ASC (Ambulatory Surgical Center) who are specifically deploying this technique : Monticelli-Vélodrome, opened since November 2016, is one of them.
To know more about ambulatory total knee arthroplasty, you could click here.
WHAT ARE THE KNEE REPLACEMENT BENEFITS ?
Once your recovery is over, you will get the following benefits :
- Reduction of your knee pain level or even total pain relief
- Higher mobility. This mobility will even be better if your knee is not too stiff before the surgery and if you are pro-active during your recovery
- More strength for your leg
- Higher quality of life
- Sport activities : you will be able to practice sport again such as walking, Nordic walking, hiking, biking, swimming, horse riding, golf,…
You will be able to practice tennis and ski again if your level of practice was good before the surgery. For tennis, you would have to prefer clay-court and double tennis.
You will have to be cautious with sports that could overload your prosthesis : avoid sports such as running or fighting sports (boxing, karate,…) that could damage your prosthesis and as such could reduce its lifetime.
TOTAL KNEE ARTHROPLASTY RISKS
Each serious surgery brings its potential risks. It is essential that you know and understand those risks before you get your surgery. Your medical team will state with you those risks when you’ll have your consultation.
Let’s state the most common risks :
Infection. This complication is pretty rare (roughly 1% of TKA cases). The bacteria contamination could occur either by the patient or by the environment. The infection could also occur way after the surgery. You’ll have to be very cautious about your personal hygiene when you’ll get a knee prosthesis.
Any types of infection, such as a dental, urinary tract, digestive, lungs, or skin infection, could lead to a prosthesis infection. Therefore, your doctor has to be aware of your TKA and has to fix all infection you could develop during your life very seriously.
Venous thrombosis - Pulmonary Embolism. To prevent this risk due to possible blood clots, your surgeon will prescribe you an anti-coagulant treatment after your surgery. Your physiotherapist will also help you to walk as soon as possible after your surgery : walking will reduce the phlebitis risk.
Haematoma. This is a normal consequence of your surgery unless this haematoma gets too big and/or it compresses tissues around your scar. Once in a great while, the haematoma will need a quick surgery to be removed.
Reflex sympathetic dystrophy. This pathology consists in a neural-digestive dysfunction. It generally occurs to patients who have a particular psychology field. This pathology can to be treated with an algology doctor with a lot of success. But it usually takes time to totally heal your neural-digestive system. This dystrophy will interfere and slow down your surgery recovery.
Other complication can occur on a very rare basis. To name few of them :
The law and medical regulations enforce your surgeon to inform the patient about all surgery risks. Knowing all these surgery risks doesn’t increase the probability of occurrence as ignoring them doesn’t reduce it.
Therefore, keep in mind that in a very broad majority, this type of TKA surgery brings significant benefits to patients when the whole medical process has been thoroughly performed.
Let’s state the most common risks :
Infection. This complication is pretty rare (roughly 1% of TKA cases). The bacteria contamination could occur either by the patient or by the environment. The infection could also occur way after the surgery. You’ll have to be very cautious about your personal hygiene when you’ll get a knee prosthesis.
Any types of infection, such as a dental, urinary tract, digestive, lungs, or skin infection, could lead to a prosthesis infection. Therefore, your doctor has to be aware of your TKA and has to fix all infection you could develop during your life very seriously.
Venous thrombosis - Pulmonary Embolism. To prevent this risk due to possible blood clots, your surgeon will prescribe you an anti-coagulant treatment after your surgery. Your physiotherapist will also help you to walk as soon as possible after your surgery : walking will reduce the phlebitis risk.
Haematoma. This is a normal consequence of your surgery unless this haematoma gets too big and/or it compresses tissues around your scar. Once in a great while, the haematoma will need a quick surgery to be removed.
Reflex sympathetic dystrophy. This pathology consists in a neural-digestive dysfunction. It generally occurs to patients who have a particular psychology field. This pathology can to be treated with an algology doctor with a lot of success. But it usually takes time to totally heal your neural-digestive system. This dystrophy will interfere and slow down your surgery recovery.
Other complication can occur on a very rare basis. To name few of them :
- Some complications are due to the surgical gesture, the anesthetist gesture or due to a technical failure or wear-out of the implant.
- Neural and vascular lesions during or after the surgery.
- Functional complications due to poor follow-up of post-surgery directions, such as too long motionless status, or knee rest interruption, or bad rehabilitation process.
- Complications due to a failure of other organs : digestive, cardio-vascular, pulmonary, skin, renal, endocrinal system, …
The law and medical regulations enforce your surgeon to inform the patient about all surgery risks. Knowing all these surgery risks doesn’t increase the probability of occurrence as ignoring them doesn’t reduce it.
Therefore, keep in mind that in a very broad majority, this type of TKA surgery brings significant benefits to patients when the whole medical process has been thoroughly performed.
HOW LONG WILL BE MY RECOVERY ?
Your surgery will take place either within the ambulatory department that will enable you to get back home the same day or within the standard surgery department and in that case you’ll stay one or 2 days at the hospital.
Your recovery time will last for roughly 2 months and will take place at your physiotherapist office.
During your stay at the hospital, you’ll get some massage and rehabilitation sessions right after your surgery. Indeed, as soon as the afternoon of your surgery, your physiologist will make you walk again. You will learn how to walk with one or two sticks, and progressively without any stick. Meanwhile your physiologist will monitor the knee flexion and knee extension progress. The same day or the day after your surgery, you will commence your stairs rehabilitation. As soon as all the Enhanced recovery after surgery (ERAS) criteria are ticked, you will be authorized to get back home.
Then, between the 4th and 6th week, you will have to reach the 90-degree flexion of your knee. If you are late getting to that number, don’t worry and make an appointment with me. I’ll control your knee and will help you to fix the painful adherence : this could be done using short anaesthesia to manipulate your knee and remove the adherences. This quick intervention will help you to catch up with your recovery program in an easy and smooth manner.
Depending on the type of your job, you’ll be able to return to business from one month after the date of your surgery. After 3 months, you’ll be able to walk without any walking stick and without any limp. At that time, you’ll be able to have more physical activities.
Then, you will get a check-up one year after your surgery. After then, your check-ups will occur every 2 years. It is essential to comply to this control process : it consists in an X-ray control with a medical consultation to monitor the evolution of your knee status.
Don’t be neglectful : this follow-up process is a key element of your long-term recovery success. This monitoring will be reported to your doctor.
Your recovery time will last for roughly 2 months and will take place at your physiotherapist office.
During your stay at the hospital, you’ll get some massage and rehabilitation sessions right after your surgery. Indeed, as soon as the afternoon of your surgery, your physiologist will make you walk again. You will learn how to walk with one or two sticks, and progressively without any stick. Meanwhile your physiologist will monitor the knee flexion and knee extension progress. The same day or the day after your surgery, you will commence your stairs rehabilitation. As soon as all the Enhanced recovery after surgery (ERAS) criteria are ticked, you will be authorized to get back home.
Then, between the 4th and 6th week, you will have to reach the 90-degree flexion of your knee. If you are late getting to that number, don’t worry and make an appointment with me. I’ll control your knee and will help you to fix the painful adherence : this could be done using short anaesthesia to manipulate your knee and remove the adherences. This quick intervention will help you to catch up with your recovery program in an easy and smooth manner.
Depending on the type of your job, you’ll be able to return to business from one month after the date of your surgery. After 3 months, you’ll be able to walk without any walking stick and without any limp. At that time, you’ll be able to have more physical activities.
Then, you will get a check-up one year after your surgery. After then, your check-ups will occur every 2 years. It is essential to comply to this control process : it consists in an X-ray control with a medical consultation to monitor the evolution of your knee status.
Don’t be neglectful : this follow-up process is a key element of your long-term recovery success. This monitoring will be reported to your doctor.
EARLY REHABILITATION WITH A TOTAL KNEE ARTHROPLASTY
This recovery technique is dedicated to specific TKA techniques that preserve soft tissues, so-called “mini-invasive” techniques. This specific technique preserving ligaments, muscles and tendons enables the Enhanced Recovery After Surgery (ERAS).
This rehabilitation protocol has been developed with the partnership of the physiologist Benjamin Thomas and the physiology center of the Frioul.
As soon as the same day of your surgery (from 4 to 6 hours after), you will stand up with the help of your physiologist. The goal is an early back home step. This goal will be achieved if the entire physiology criteria are validated. These criteria, reached within the first days after your surgery, are explain hereunder.
Therefore, it is mandatory that you are fully armed to perform your first rehabilitation phase: bring your crutches and shoes (sneakers are OK) with you at the hospital. You won’t have any drains or any perfusion equipment. As such, your medical team will advise you to wear baggy clothes. You will have diner at your table and not in your bed. So, bear in mind : you are not sick, you’ve just got a surgery.
The early back home step is essential for your fast and smooth recovery. These new and innovative care pathways enable seamless rehabilitation and generate less post-surgery risks.
At that stage, there are 5 criteria to be validated :
This rehabilitation protocol has been developed with the partnership of the physiologist Benjamin Thomas and the physiology center of the Frioul.
As soon as the same day of your surgery (from 4 to 6 hours after), you will stand up with the help of your physiologist. The goal is an early back home step. This goal will be achieved if the entire physiology criteria are validated. These criteria, reached within the first days after your surgery, are explain hereunder.
Therefore, it is mandatory that you are fully armed to perform your first rehabilitation phase: bring your crutches and shoes (sneakers are OK) with you at the hospital. You won’t have any drains or any perfusion equipment. As such, your medical team will advise you to wear baggy clothes. You will have diner at your table and not in your bed. So, bear in mind : you are not sick, you’ve just got a surgery.
The early back home step is essential for your fast and smooth recovery. These new and innovative care pathways enable seamless rehabilitation and generate less post-surgery risks.
PHASE 1 : starting the day of your surgery
You will exit the surgery room without any drain. A contention bandage will be set on your leg and will be removed day 2.At that stage, there are 5 criteria to be validated :
- Be able to stand up from your bed and lay down in your bed by your own
- Locking your knee when it is outstretched
- A 90 degrees flexion of your knee
- Be able to walk by your own, with or without crutches and without any splint
- Going upstairs and downstairs
PHASE 2 : starting at your physiologist office
- Patella passive manipulation
- Passive manipulation with flexion/extension movements (manual, laid down, sit down at the edge of the bed), learning of the self-rehabilitation while seated
- Locking your knee when you are laid down (crush a cushion)
- Full weight bearing walking
- Walking upstairs and downstairs
- Get rehabilitation advices
SELF-REHABILITATION PROGRAMS
These self-rehabilitation programs were developed in collaboration with Dr Jérôme Villeminot.
KNEE PROSTHESIS SELF-REHABILITATION
KNEE PROSTHESIS SELF-REHABILITATION




